What are muscle and tendon injuries?
Muscles and tendons are the tissues that move joints. The muscles are the “red meat” of the body. When they receive a signal from the brain via the nerves the muscles contract i.e. shorten and bunch. The pull is transmitted through the tendon to the bone on the far side of the joint so the joint moves. Muscles and tendons can tear through overloading e.g. lifting too much or can be cut or crushed from outside.
What do they look like?
Muscle and tendon injuries are often obvious because of local pain and swelling. Initially the injury may be underestimated as patients’ are often reluctant to remove local joints when they are sore from injury. Joint movement should return within days if the muscle/tendon is intact. Particularly if there has been a cut then if there is doubt the area should be explored under anaesthetic, probably in an operating theatre by an experienced surgeon.
How is the diagnosis made?
The Hand specialist who sees the patient will ask questions about their injury and in particular how it occurred. They will then examine the patient looking at the injured site. In particular they will look at movement of local joints. The Hand specialist will compare the passive movements, i.e. how much the joint can be move by someone else, with the active movements i.e. how much the patient can move their own joint.
What investigations (tests) are needed?
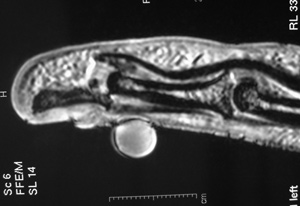
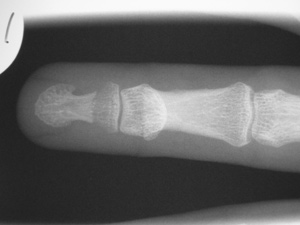
For the milder injuries no tests are needed. For most of the rest of the injuries X-rays will be performed. Most of the injuries show nothing on the X-rays. Sometimes a bone fracture will show it the tendon has torn out of its attachment to bone. If there is a large fracture fragment which can occur this is usually treated as a bone injury (see fracture handbook). If there has been a cut with a dirty implement or a crush injury foreign material may be shown on the X-ray. Sometimes if the injury is still unclear an ultrasound scan (as used for pregnant women) or an MRI scan may be requested. Other tests such as a CT scan may be ordered to assess the bones and joints if there are concerns about associated injuries at the same site.
MRI scan: An MRI scanner is usually a short tunnel which the patient’s arms and top half of the body go into. Usually the arms are stretched out in a “superman” pose which is a little uncomfortable but generally well tolerated. Once in the tunnel a loud magnet is spun around and images of the bones and soft tissues created. Some people find the tunnel rather claustrophobic. If any patient doubts whether they would tolerate the scan they are best advised to visit the scanner department in advance. The films will be reported by a radiologist but also reviewed by the Hand specialist who will advise the patient accordingly.
CT scan: A CT (or CAT) scanner is a short large open tunnel. The patient lies on a bed and passes through the tunnel whilst X-rays are shone from various directions at the area of the body being investigated. It is particularly useful for showing bone abnormalities but less good at investigating soft tissue problems. The films will be reported by a radiologist but also reviewed by the Hand specialist who will advise the patient accordingly.
What treatment is needed?
If the muscle/tendon injuries are partial (incomplete) then rest and supervised movement are often sufficient for a very good recovery. The muscle/tendon needs to be protected for at least 6 weeks and as much as 12 weeks for heavy activities. If the tear or cut is complete than in most cases surgery would be recommended otherwise there will be significant weakness and possibly disability.
Surgery is performed under anaesthetic in an operating theatre. For injuries in the hand and fingers surgery can often be performed under local anaesthetic. Injuries further up the arm and in children typically require a general anaesthetic as do extensive i.e. multiple tendon injuries. Muscle repair is difficult as the tissues do not hold stitches (sutures) well. The repairs are therefore not very robust and need protection typically for 4-6 weeks initially and for 12 weeks for heavy activities. Tendon repairs are usually more robust but tendons heal more slowly so need protection. But they also tend to stick down to local tissues so they need to be moved early starting within days of the repair. This movement needs to be carefully controlled and protected. This is performed protected by a splint and supervised by the treating team and Hand therapists.
Injuries to the bending tendons of the fingers are particularly prone to failure or to sticking down because the track in which they run is so narrow. The period of post-operative therapy requires particularly close supervision for the first 5 weeks and care for up to 12 weeks.
What happens in the next few weeks?
The care of the hand in the post-injury/post-operative period is very important in helping to ensure a good result. Initially the aims are comfort and elevation.
Comfort and elevation: These are met by keeping the hand up (elevated) especially in the first few days and by use of a long acting local anaesthetic (Bupivicaine) if the hand/wrist/elbow has been operated upon. The local anaesthetic lasts at least 12 hours and sometimes 48 hours. Patients should start taking painkillers before the pain starts i.e. on return home and for at least 24 hours from there. This way most of our patients report little or any pain.
Dressings: Muscle and tendon repairs need dressing for 10-14 days until the wounds are healed. The repairs almost always need protection and usually careful early movement for 4-6 weeks as noted above.
Movement: Most joint movement should be regained gained following surgery in the arm and wrist especially if only one or two muscles/tendons are injured. For more complex injuries and particularly for tendon repairs in the fingers there will be some long-term stiffness especially in the finger PIP joints. Most movement occurs in the first 6-12 weeks (especially the first 6 weeks in the fingers). This time must be used productively to ensure a good result. The key is regular long gentle stretches both into straightening and into bending. Ideally these should be performed for 5 mins in each direction (feeling the stretch but without pain) once an hour. In practical terms most people manage to stretch 5-6 times a day. Elevation and icing the elbow also help reduce swelling and thus pain and improve movement. The movements will be taught and supervised by the treating specialists and Hand therapists but as with all therapy the patients have to do the work guided and encouraged by the treating specialists and therapists.
Wound massage: Once the wound(s) have healed (typically after 2 weeks, or after 4-6 weeks if protected in plaster) they should be massaged by the patient 3 times a day with a bland soft cream for 3 months. This reduces the scar sensitivity and adherence which can be a nuisance. If this is marked hand therapy may be organised to help reduce the scar tenderness but this is rarely required. Patients should avoid pressing heavily on the scar for 3 months following the operation as this will be quite painful. Examples of activities to avoid are using the palm to grip/twist a heavy or tight object or use the palm to help get out of a chair.
Return to daily activities: The hand can be used for normal activity following surgery only after the first 4-6 weeks. Most patients can drive a few days after stopping using the splint full-time but should be guided by the treating team. Most patients take at least 4-6 weeks to return unless it is very light office work; return to heavy manual work may take up to 2-4 weeks even for mild injuries and typically 9-12 weeks or so following surgery. The treating team should advise about this.
What are the results of treatment?
Most patients heal without significant problems especially for mild injuries. For more severe injuries particularly if surgery is required then full recovery is infrequent. In the arm and hand the term “functional range of movement” is widely used. This means a range of movement adequate for 90% of daily activities (assuming the other joints are normal). For each of the elbow, wrist and hand the ranges for good function are typically:
Elbow – 30–1200 i.e. nearly but not fully straight by 300 and bending well but not fully. The normal range of movement is 0-1400
Forearm – 45-450 i.e. just over half of normal movement. The normal range is supination (turning the palm up) 800 and pronation (turning the palm down) 750
Wrist – Extension (cocking the wrist back) 300 and flexion (bending the wrist down) 100. This is around 25% of normal movement which is extension of 800 and flexion of 800
Thumb
MP joint – Fixed flexion deformity of 100 and flexion to 300. Normally the range is very variable between individuals. Stiffness in this joint is well tolerated if the joint is painless and stable.
IP joint – Fixed flexion deformity of 100 and flexion to 300. Normally the range is very variable between individuals. Stiffness in this joint, like the MP joint is well tolerated if the joint is painless and stable.
Fingers
MP joint – Fixed flexion deformity of 100 and flexion to 400. Normally the range is 0-900. Stiffness in this joint is better tolerated than in the PIP joint (see below). In general loss of flexion (bending) is better tolerated than loss of extension (straightening).
PIP joint – Fixed flexion deformity of 300 and flexion to 800. Movement in the PIP joints is very important and stiffness is not well tolerated. The normal range of movement is 0-1100
DIP joint – Fixed flexion deformity of 100 and flexion to 300. Normally the range is 0-700. Stiffness in this joint, like the IP joint of the thumb is well tolerated if the joint is painless and stable.
Most of these ranges are achieved but not always especially with injuries to multiple tendons, injuries to the bending tendons in the fingers and combined injuries such as tendon as well as nerve/bone/artery injuries. Most patients have long-term aching in the cold but this may improve for up to 3-4 years from injury and in usually not too marked. Secondary reconstructive surgery is required in about 10% of patients being more common in patients with more complex injuries and injuries to the bending tendons in the fingers.
Are there any risks from surgery?
All interventions in medicine have risks. In general the bigger the operation the greater the risks. With injuries the outcome is mainly due to the severity of the initial injury. For muscle/tendon repairs the risks include:
- The scar may be tender, in about 20% of patients. This usually improves with scar massage, over 3 months.
- Aching at the site may last for several months and possibly for ever.
- Grip strength can also take some months to return to normal if ever.
- Stiffness may occur in particular in the fingers.
- Numbness can occur around the scar but this rarely causes any functional problems.
- Wound infections occur in about 1-5% of cases. These usually quickly resolve with antibiotics.
- Chronic Regional Pain Syndrome “CRPS”. This is a rare but serious complication, with no known cause or proven treatment. The nerves in the hand “over-react”, causing swelling, pain, discolouration and stiffness, which improve very slowly.
- Any operation can have unforeseen consequences and leave a patient worse than before surgery.