Solid Lumps in the Hand
What are solid lumps in the hand?
These are common conditions caused by mistakes in the turnover of normal cells in the hand. They are almost always benign but sinister lumps (cancer) can occur (although < 1% of hand lumps are cancerous). The typical symptoms are of a slow growing painless lump in the hand, most commonly a finger, that comes on for no obvious reason. As the swelling enlarges it can become a nuisance with daily activities. Lumps at the bottom of the fingers and in the palm mainly cause problems with gripping. Lumps at the ends of the fingers tend to cause awkwardness with fine activities. The lumps tend to be solitary, i.e. not associated with lumps elsewhere. Rarely there will be some numbness or pain associated with the swelling.
Types of lumps
The lumps are made up of whatever tissue in the hand has malfunctioned (see below).
The main types are: Giant cell tumour; Lipoma; Fibroma; Neuroma and Various Others.
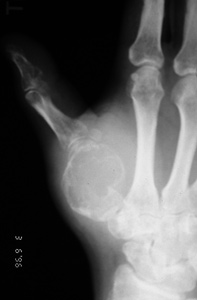
Giant cell tumour
This is the commonest solid lump in the hand. It is made up of cells from the lining of the tendon sheath or joint capsule. Despite its powerful sounding name it is benign i.e. only a local problem and does not spread elsewhere.
Lipoma
This is a lump made up of fat cells. It is very common in the body in general especially around the trunk but not in the hand.
Fibroma
This is a lump made up of fibrous cells. It is typically on or just below the surface of the skin. It is more commonly associated with an injury.
Neuroma
This is a lump made up of nerve cells. There are 2 main subtypes: the true neuroma made up of true nerve cells. This mainly occurs following an injury and is often associated with local pain and numbness; and the schwannoma made up of cells that surround the nerve. This is usually painless.
Various Others
These include lumps due to calcification, gout, blood vessels (calles haemangioma) bone prominences associated with arthritis and Dupuytren’s disease (a common inherited benign disease – see separate information sheet).
Why do they occur?
Normally cells in the body turnover on a daily basis. They are programmed to maintain equilibrium i.e. stop multiplying when there are enough of them. Errors occur in this process and the cells continue to grow. How frequently this occurs is not known. Probably most of the tine this occurs the body deals with it on its own. If it fails a swelling occurs and grows locally. If a major malfunction occurs then a cancerous growth appears and may spread. Almost all growths in the hand are NOT cancerous. There is limited space in the hand and as the lump enlarges it becomes more prominent and more of a nuisance. Benign lumps in the hand almost never become cancerous.
What happens if nothing is done?
(This is referred to as the natural history i.e. what happens if Nature runs its own course.). In almost all cases the lumps will slowly enlarge both becoming more of a nuisance and being more difficult and thus more risky to remove surgically.
Making the diagnosis
The Hand specialist who sees the patient will ask questions about their symptoms, when they started, how they progressed, what treatment (if any) they have had and other questions relevant to the problems. They will then examine the patient looking at the wrists and hands and in particular. If there is a possibility it is a cyst (see information sheet) they may try to shine a small torch through it.
What test(s) might be performed?
Tests (also known medically as Investigations) include X-rays, scans, blood tests and particularly in the hand electrical tests (known as EMGs or Neurophysiology). These may be used to help make or confirm a diagnosis after a patient has described their symptoms and been examined.
With solid lumps in the hand the diagnosis is usually obvious after listening to and examining a patient. Occasionally the Hand specialist will request an MRI scan to show the extent of the lump particularly if it is large. This helps plan the operation rather than making a definitive diagnosis which requires surgery. An MRI scanner is usually a short tunnel which the patient’s arms and top half of the body go into. Usually the arms are stretched out in a “superman” pose which is a little uncomfortable but generally well tolerated. Once in the tunnel a loud magnet is spun around and images of the bones and soft tissues created. Some people find the tunnel rather claustrophobic. If any patient doubts whether they would tolerate the scan they are best advised to visit the scanner department in advance. The films will be reported by a radiologist but also reviewed by the Hand specialist who will advise the patient accordingly.
If there is a chance the lump may be a cyst (see information sheet) the Hand specialist may attempt to suck out fluid from it with a needle (aspiration). This is performed under local anaesthetic.
Treatment:
What are the non-operative treatments?
The options are either to do nothing accepting that the lump will slowly enlarge and one day need treating, or plan surgical excision. No non-operative treatments such as drugs or diet will alter the lump.
What does the operation involve?
The operation is called excision of mass in the hand. The operation is almost always performed under local anaesthetic. It is performed with a bloodless field by use of a tourniquet either as a band, like a blood pressure cuff, placed around the top of the arm for hand swellings or a small band placed around the base of the finger for finger swellings. The arm band is inflated (tightened) during the operation to reduce bleeding, which makes the operation easier and safer. It can be a little uncomfortable, but is almost always well tolerated for the 10-20mins or so that it is inflated (this happens just before the surgeons starts the operation). Base of finger tourniquets are painless as the finger is numb. Before that the arm is painted with an antiseptic with a pink dye in it. This is used to help minimise the risk of infection.
The lump will be removed, typically through a zig-zag incision, as straight longitudinal incisions on the palmar surface of the hand often lead to contractures. Swellings on the back of the hand, however, are usually better removed by a straight longitudinal incision unless they are very small, when a transverse incision may be employed, as this is cosmetically a little better. The important neighbouring structures, particularly the nerves and arteries, will be identified and preserved. They can be very close to the lump and at risk of injury so this is not an operation for the occasional surgeon but should be performed by a reasonably experienced hand surgeon. The swelling will be removed and will be sent to the Laboratory for analysis, as is standard. The skin is usually sewn up with absorbable stitches. A supportive dressing is applied and the patient’s arm elevated.
The total time in hospital is usually 1-2 hours.
What happens in the next few weeks?
The care of the hand in the post-operative period is very important in helping to ensure a good result. Initially the aims are comfort and elevation. These are met by keeping the hand up (elevated) especially in the first few days and by use of a long acting local anaesthetic (Bupivicaine). The local anaesthtic lasts at least 12 hours and sometimes 48 hours. Patients should start taking painkillers before the pain starts i.e. on return home and for at least 24 hours from there. This way most of our patients report little or any pain.
The bandage can be removed after 2-7 days, leaving a sticky dressing beneath. The patient or GP practice nurse can do this. If well healed at that stage then the wound can be left open (exposed). If in doubt it can be covered with a light dressing for a few more days. The patient is reviewed in clinic between 2-4 weeks following the operation. Typically dissolvable stitches are used so they should not require to be removed.
The hand can be used for normal activity after the first few days. Most patients can drive after a 3-5 days. Most patients return to work in 5-7 days, but this varies with occupation; heavy manual work usually takes several weeks. The wound should be massaged by the patient 3 times a day with a bland soft cream for 3 months once the wound is well healed (typically after 2 weeks). This reduces the scar sensitivity which can be a nuisance. If this is marked physiotherapy may be organised to help reduce the scar tenderness but this is rarely required. Patients should avoid pressing heavily on the scar for 3 months following the operation as this will be quite painful. Examples of activities to avoid are using the palm to grip/twist a heavy or tight object or use the palm to help get out of a chair.
What are the results of the operation?
At least 90% of patients in studies say they have a good or excellent result following this operation, with resolution of the swelling
Are there any risks?
All interventions in medicine have risks. In general the larger the operation the greater the risks. For removal of benign solid lumps in the hand the risks include:
- The scar may be tender, in about 20% of patients. This usually improves with scar massage, over 3 months.
- Aching may occur for several weeks but usually settles fully. Grip strength can also take some months to return to normal.
- Stiffness may occur in particular in the fingers. This is usually short-term and only infrequently requires physiotherapy. But it is very important that it is resolved quickly to avoid permanent stiffness. This occurs rarely but can do associated with CRPS (see below)
- Numbness can occur around the scar but this rarely causes any functional problems. Numbness at the important end of the finger is rare (<1%) in out practice.
- Wound infections occur in about 1% of cases. These usually quickly resolve with antibiotics.
- Chronic Regional Pain Syndrome “CRPS”. This is a rare but serious complication, with no known cause or proven treatment. The nerves in the hand “over-react”, causing swelling, pain, discolouration and stiffness, which very slowly improve.
- Any operation can have unforeseen consequences and leave a patient worse than before surgery. This is rare for removal of solid lumps.